
As the number of COVID-19 cases and associated deaths continue to rise, affecting people of all ages, the importance of staying home and practicing physical distancing is becoming increasingly clear. Yet one question continues to linger in some people’s minds: does recreating at the beach really increase my risk of getting sick with COVID-19?
The policies regarding outdoor recreation vary by state and, at times, even by jurisdiction. Some areas have closed all beaches and are strictly enforcing stay-at-home orders, while other areas are still allowing people to get outside and recreate as long as physical distance is maintained. Due to the highly infectious nature of the SARS-CoV-2 virus (referred to here as the COVID-19 virus), the Surfrider Foundation and numerous other outdoor recreation groups have encouraged supporters to stay home to avoid contributing to the spread of the virus.
As of May 2020, Surfrider is supportive of thorough coastal recreation plans that outline strong physical distancing requirements and other protocols to minimize the risks outlined below, while allowing for safe coastal recreation in areas that are starting to open beaches; however, public health remains a priority and if guidelines are not followed, health experts warn that transmission rates will increase and could cause the re-instatement of at-home orders and beach closures.
In terms of potential COVID-19 risks at the beach, what does the latest science tell us? Here’s what we’ve been able to find from the available scientific literature and discussions with leading experts in the field. Please note that the COVID-19 virus is new and much of the current research is based on how similar coronaviruses behave. As research specific to COVID-19 is rapidly emerging, the science is subject to change as we learn more.
Will following the 6-foot physical distancing guideline keep me safe?
The CDC has long stated that large droplets released during a cough, sneeze or even an exhalation can travel up to six feet. This finding is the basis for the national 6-foot physical distancing recommendation during the COVID-19 pandemic, as well as for other disease prevention efforts including the flu. However a new study by Dr. Lydia Bourouiba from MIT has found that droplets carrying an infectious virus can travel much farther, up to a distance of 23 to 27 feet. When we sneeze, cough or exhale, droplets and aerosols can be released in what’s referred to as a “turbulent gas cloud.” This cloud provides the right humidity and momentum to propel both large droplets and small aerosols farther and for a longer period of time (the collective humidity of the cloud reduces the rate of evaporation that would otherwise happen within seconds).
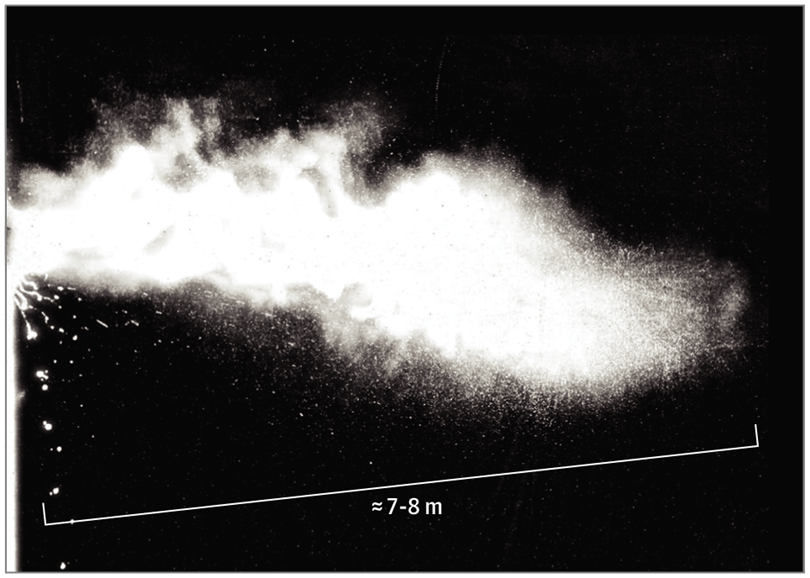
“Multiphase Turbulent Gas Cloud From a Human Sneeze.” Image from Dr. Bourouiba’s paper published on JAMA.
As such, Dr. Bourouiba concludes “recommendations for separations of 3 to 6 feet (1-2 m) may underestimate the distance, timescale, and persistence over which the cloud and its pathogenic payload travel, thus generating an underappreciated potential exposure range for a healthcare worker.” She then encourages healthcare workers to wear proper protective gear even farther than 6 feet from an infected patient. These concerns regarding additional spread and transmission risk through aerosols were further supported in a May 27 paper by Dr. Kim Prather et al, where people are encouraged to wear masks indoors even with 6 feet distancing. In other words, if an infectious dose is able to travel longer distances, staying 6 feet away from other people may not be far enough to protect us from the COVID-19 virus. Though this risk is considered lower for outdoor environments, as Dr. Prather states “breezes and winds often occur and can transport infectious droplets and aerosols long distances. Asymptomatic individuals who are speaking while exercising can release infectious aerosols that can be picked up by air streams. Viral concentrations will be more rapidly diluted outdoors, but few studies have been carried out on outdoor transmission of SARS-CoV-2”. A recent study tracking COVID-19 cases in China found only one confirmed instance of an “outdoor outbreak” in which the virus was transmitted during an outdoor discussion between neighbors. For now, health experts suggest the more distance you can put between yourself and others, the better. With so many asymptomatic cases, and the long time period between when someone becomes infectious with the disease and when they start to show symptoms, we really can’t tell who is healthy and who poses a severe risk.
Can’t I just wear a face mask when I’m at the beach?
As of Friday, April 3, the federal government has shifted their guidance and is now recommending that everyone wear face masks when in public to help reduce the transmission of the disease. The act of wearing a mask is intended to prevent people who may not realize they are infected with COVID-19 from spreading the virus when coughing, sneezing or exhaling. While surgical masks are more effective at reducing the release of droplets and aerosols when worn by infected individuals, cloth masks may still help prevent infected droplets from being released. As such, wearing cloth masks could help reduce the spread of the virus when worn correctly and widespread. FDA warns that cloth masks are not protective and should not be relied upon to keep you safe when in public or close proximity to others; however, recent study results (see Konda et al and Ma et al) indicate that homemade cloth masks made with multiple layers and material combinations may be effective at protecting the mask wearer if worn correctly (no gaps between skin and the mask). Due to varying degrees in efficacy of homemade masks and high instances of improper wearing practices, maintaining distance is still key for protecting individuals from COVID-19, even when wearing a mask. The CDC provides guidance on homemade cloth face coverings and requests that people avoid the use of N95 masks which should be reserved for healthcare workers.
Can the virus spread through contaminated beach sand, structures and facilities?
The potential transmission route from touching contaminated surfaces is the basis for the CDC recommendation about not touching your nose, eyes or mouth with unwashed hands. This is because various studies are finding that these infectious droplets can land and settle on nearby surfaces and remain infectious for a period of time (up to three days or more on hard, non-porous surfaces like plastic and steel). If someone touches that contaminated surface and then touches their eye, nose or mouth, they may be able to contract the disease. Therefore, at the beach, if an infected individual coughs, sneezes or even breathes on handrails, bathroom stalls, toilets, or other structures and facilities, those surfaces can become contaminated and potential transmission sources for other beachgoers. At this point, there is no literature available about contaminated sand being a potential transmission route.
Can I get sick with COVID-19 from swimming in contaminated beach water?
Researchers from a recent Water Research Foundation webinar stated that the virus has been shown to remain viable and infectious, at least temporarily, in natural freshwater environments including lakes and streams. While dilution is suspected to keep the risk low, researchers note that high concentrations of the viable COVID-19 virus could put freshwater recreation users at risk. There is still no information on the ability of the COVID-19 virus to remain viable in saltwater, so it’s unclear if swimming at saltwater beaches elevates the risk of getting sick. Learn more about COVID-19 and beach water quality here.
Can the virus spread through sewage?
Like many harmful viruses and pathogens, a main exposure risk to the water recreation community is from sewage pollution. The release of raw or undertreated sewage into our surface waterways can cause diseases to spread through the “fecal-oral transmission route.” In other words, when we recreate at the beach during a sewage spill or release of undertreated wastewater, we risk ingesting fecal-borne pathogens that can cause symptoms such as stomach upset; ear, eye, nose and throat infections; as well as more severe infections like E. coli, MRSA, giardia, hepatitis, and worse.
At this point, the research community does not know if people can contract the COVID-19 virus from exposure to feces in recreational waters but the overall consensus is that it might be possible. The RNA of the virus was found in stool samples of infected patients, and some researchers are even exploring the potential to track COVID-19 cases by testing for virus’ RNA in raw sewage (practicing “sewage surveillance”) before it gets treated at sewage treatment plants.
We currently do not know if the virus remains infectious after passing through the human digestive system, and the findings to date are mixed. In order to be infectious, the virus needs both intact RNA and an intact outer envelope. A preliminary study out of Germany determined that the outer envelope is not able to remain intact after passing through the digestive system. Alternatively, a recent research letter mentions that a study from China found the live, infectious COVID-19 virus in the stool of two patients, but experts note that this was just initial evidence from a small sample, and requires further investigation. Another study out of China determined that “[t]he continuous positive detection of viral RNA from feces suggests that the infectious virions are secreted from the virus infected gastrointestinal cells.” The authors infer that this finding implies that the virus is infectious in stool, yet an actual intact outer envelope was not identified.
There is also reporting that speculated on the potential for the virus to become aerosolized in sea spray when polluted waterways are actively churned or agitated (such as when a wave breaks), but this is currently unsubstantiated and just speculative since we don’t know if the virus is infectious in raw sewage, or how it behaves after “exposure to air, sunlight, and water”. This concern was also discussed on an April 16 webinar from the Water Research Foundation, where researchers note that while the risks of getting sick with COVID-19 from exposure to polluted coastal aerosols are still unknown, untreated wastewater and sewage could include other substances beyond feces, such as saliva and mucus carrying the infectious COVID-19 virus, which may pose a risk to coastal recreators. But yet again, additional research is needed to confirm. Specific to aerosolized sewage, previous concerns were voiced in a 2009 study regarding the 2003 SARS-CoV outbreak, a virus closely related to the COVID-19 virus. Authors mention an instance where SARS-CoV “was spread when water contaminated with fecally shed virus was inhaled, causing respiratory infection” due to a faulty plumbing system in a Hong Kong apartment building.
The potential for sewage to contain the infectious COVID-19 virus is of particular concern to areas that experience persistent spills and releases of raw sewage, such as coastal communities along the US/Mexico border. Since infected individuals are able to shed the virus in their stool for up to five weeks after recovering from the disease, additional research is needed to confirm the potential for sewage to act as a transmission route. A proposed study to determine if the infectious COVID-19 virus is present in sewage-polluted coastal water and able to aersolize in sea spray, submitted by Dr. Kim Prather from Scripps Institution of Oceanography, was recently awarded funding by the National Science Foundation. The study is scheduled to start immediately (this week), but won’t be completed until March of next year. In the meantime, researchers from last month's Water Research Foundation webinar stated that the “likelihood of catching COVID-19 from feces seems low” since other coronaviruses are susceptible to UV radiation and unable to persist over long periods of time in waterways. However this is just preliminary and additional studies are needed to help clarify the potential for this transmission route.
Do sewage treatment plants eradicate the virus?
Typical wastewater treatments that include sterilization with chlorine and other disinfectants are expected to be highly effective at eradicating the virus. That said, there has been a recent push to test which sewage treatment mechanisms are most effective at eradicating the COVID-19 virus. Additionally, if you are in a place that uses only primary treatment at your sewage treatment plant, which includes separation of liquids from solids without disinfection, it could be possible that the viable virus might be discharged with effluent into waterways through offshore outfalls or groundwater injection wells. Researchers from the Water Research Foundation webinar noted some concern about biosolids, which are waste solids from treatment plants used as fertilizer, being able to accumulate viruses and other pathogens if not treated to Class A standards, but no literature was provided to confirm this potential risk. In the meantime, to keep wastewater systems functioning properly and therefore prevent potential raw sewage exposure to maintenance staff, the EPA asks that people flush only toilet paper (no flushable wipes!) and avoid dumping grease down drains. Conserving water in your home and minimizing the amount of water that goes down the drain also helps keep wastewater systems from being overloaded. You can find helpful water conservation tips here.
Key takeaways
While there are still a lot of unknowns about the COVID-19 pandemic, it’s clear that we need to proceed with caution. The science to date tells us that recreating at the beach, and other frequently visited public areas (including parks, trails and more), could put you at higher risk of getting sick when compared to practicing self isolation and sheltering in place. However, review of case studies indicates that outdoor air transmission of the virus is not as likely or risky as indoor transmission, but caution should still be taken to keep physical distance from others. Potential transmission routes include inhaling contaminated droplets transmitted through the air (though this is considered lower risk in outdoor environments); touching contaminated surfaces like railings, parking meters or toilets; or swimming in sewage-contaminated waters. Even if sewage is determined not to contain the viable COVID-19 virus, exposure to sewage when swimming at the beach will put you at risk to a long list of other, harmful diseases and pathogens. Please note that much of the research is preliminary and additional studies are needed to confirm coastal transmission routes, but for now, based on the information currently available and large amounts of uncertainty, the best way to stay safe during the COVID-19 pandemic is to physically distance yourself from others.
To learn more about best practices for keeping yourself, your family and your community safe, be sure to visit the CDC COVID-19 website, and follow local, state and federal policies and recommendations.
